Heart of a Giant Foundation
Improve Early Detection, Diagnosis, and Support of Cardiac Risk Factors in High-Risk Populations. By Donating Today!

HGF
About Heart of a Giant Foundation
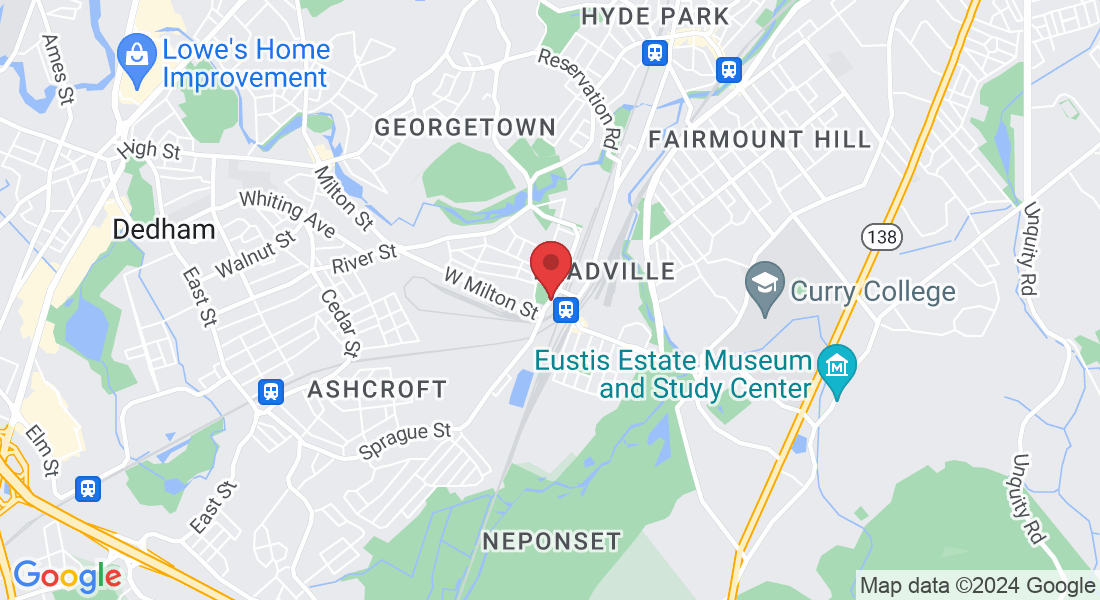
Heart of a Giant Foundation (HGF) is a Boston-based nonprofit organization dedicated to improving the early detection, diagnosis, and support of cardiac risk factors in high-risk populations.
HGF was founded by Somaneh “Bouba” Diemé. Bouba has been dealing with congestive heart failure, a condition related to his congenital heart disease, for 10 years. Recently, he underwent a heart transplant and made a strong recovery.
OUR PROGRAMS
Donate Today or Get Involved
Our work applies proven and innovative approaches to promote healthy living, prevent chronic diseases, and improve health outcomes. All applicable program elements are HIPAA compliant. Our programs support the full spectrum of patient care, from awareness-raising, education to care support.
Get Involved
We strive to be the premier partner for the early detection, diagnosis, and support of cardiac risk factors in high-risk populations.
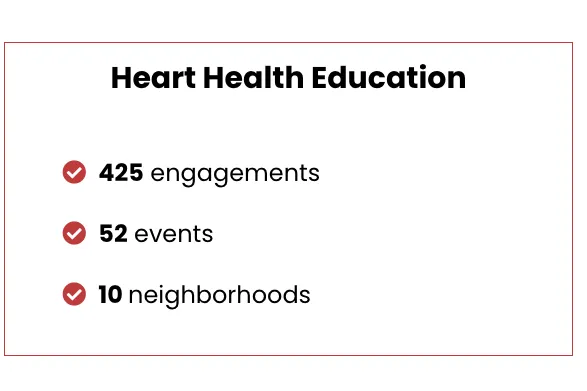
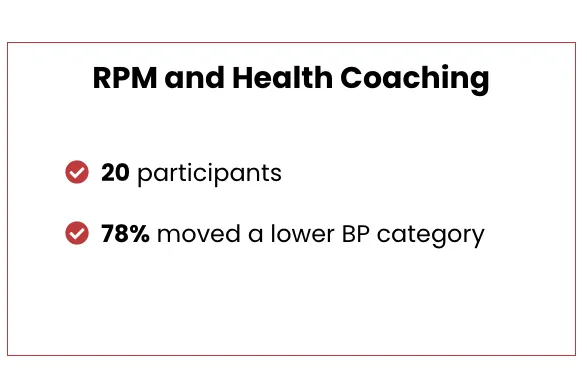
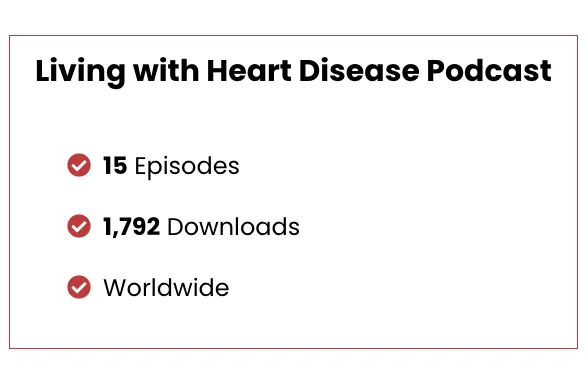
Our 2023 Numbers
How You Can Help
Help save lives and make an impact by raising funds for HGF. Host events, start campaigns or get creative to raise awareness and support. Make a difference today!
Volunteer for a great cause and make a difference. Your time and resources matter. Get involved and create an impact.
Please consider donating to Heart of a Giant Foundation to make a direct impact. Visit the website for details.
Advocate for heart donation. Spread awareness through social media, letters, and advocacy. Save lives.
News and Insights
Disclaimer:
The information shared on this page is not intended to replace professional medical advice. Always consult with a healthcare provider for any medical issues.
Consultant Local Étude Mali
Consultant local pour la conduite de réunions avec les parties prenantes sur les maladies non transmissibles (MNT) au Mali. ...more
careers
May 02, 2024•2 min read
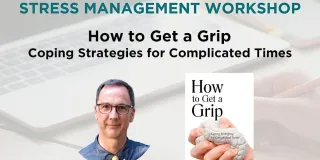
Online Workshop: Coping Strategies for Complicated Times
We at Heart of a Giant are delighted to invite you to a Stress Management Workshop led by Milton resident Dave Bullis, PhD. ...more
Event
March 27, 2024•1 min read
Book Presentation: Coping Strategies for Complicated Times
We at Heart of a Giant are delighted to invite you to our Milton neighbor, Dave Bullis, Ph.D. Book Presentation titled "How to Get a Grip: Coping Strategies for Complicated Times." ...more
Event
March 27, 2024•1 min read
Testimonials
The Heart of a Giant Foundation, Inc. is a 501(c)(3) nonprofit organization, EIN 84-2900386. Donations are tax-deductible.